TRANSCRANIAN ENDOSCOPIC APPROACH IN A FRONTAL POLYPOSIS
Abstract: Va prezentam cazul unui pacient in varsta de 62 de ani cu o formatiune tumorala voluminoasa de sinus frontal bilateral, sindrom cefalalgic sever si distructia parcelara a laminei papiracee stangi si a peretelui posterior al sinusului frontal drept.
Abordul endoscopic s-a efectuat printr-o fereastra intersprancenoasa de mici dimensiuni, cu refacerea suportului osos la finalul interventiei utilizand un mash din titan.
Desi echipa chirurgicala are o experienta indelungata in abordul transnazal endoscopic, exista cazuri in care parcursul transnazal nu poate rezolva in deplina siguranta anumite patologii. Autorii doresc sa sublinieze necesitatea utilizarii unui abord care sa asigure managementul corespunzator al unor eventuale complicatii intraoperatorii specifice acestor tumori (sangerari, fistula LCR) si in cazul de fata, abordul endoscopic transcranian a reprezentat cea mai buna solutie.
Cuvinte cheie: sinus frontal, tumori, abord endoscopic extern
Abstract: We present the case of a 62 year-old patient with a large bilateral frontal sinus tumor, severe headache and a partial destruction of the left papyracea lamina and the posterior wall of the right frontal sinus.
The endoscopic approach was performed through a small bone window by the midline of the glabella, with the restoration of the bone support at the end of the surgery using a titanium mash.
Although the surgical staff has a lot of experience in doing the endoscopic trans-nasal approach, there are some cases where the trans-nasal route cannot safely solve certain pathologies. This is the reason why the authors wish to illustrate the need of using an approach that will ensure a proper management of any kind of complications that can occur during surgery, specific to these tumors (bleeding, CSF leak). In this case, the transcranial endoscopic approach was the best solution.
Keywords: frontal sinus, tumors, external endoscopic approach
62 year-old patient, S.I, comes at our hospital with an intensive headache syndrome treatment-resistant, which had been known for several years and had worsened in the last 2-3 weeks. Three years ago (05.2016), in another ENT service, the patient underwent a curative surgery for bilateral fronto-ethmoido-sphenoidal rhinosinusitis. According to the medical discharge presented by the patient, the frontal sinus approach used was of the Draf I kind, without exploring the frontal sinus cavity.
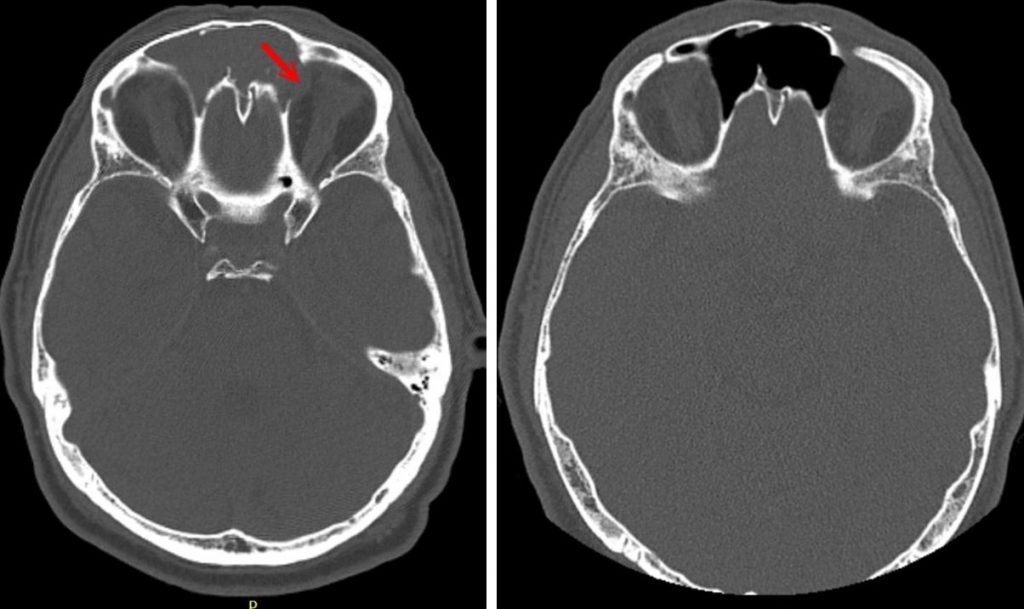
The CT / MRI scans on admission revealed the existence of a tumor-like formation, with intense gadolinium (hypercaptant), that had ballooned both frontal sinuses, and destroyed the intersinusal wall. Prolonged evolution led to a lysis of a wall caused by a decubitus injury. This explained the intimate tumoral contact with the dura mater through an 8 mm bone breach in the posterior wall of the right frontal sinus. Also, the tumor protruded through the left orbit by an erosion of the left papyracea lamina, with the appearance of a discrete inferior and external exophthalmia in the left eye. The MRI revealed that the dura mater was integral and the orbital periosteum was apparently free (fig. 1).
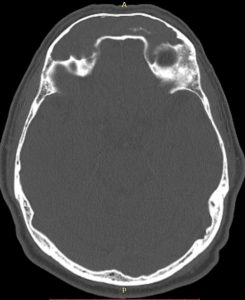
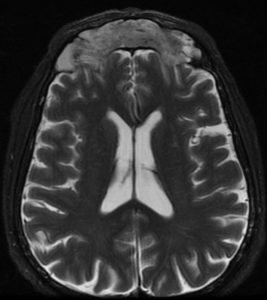
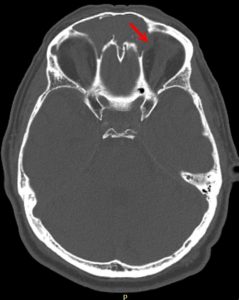
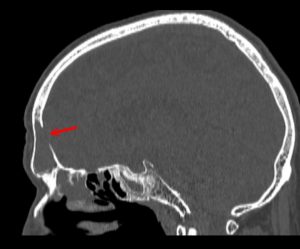
Fig 1. Up: CT and MRI T2 FSE axial preop.
Down: partial destruction of the left eye papiraceea lamina, bone breach to anterior cerebral
The apparent origin located at the posterior wall of the bilateral frontal sinus, the partial exposure of the dura mater and the destruction of the lamina papyracea with the penetration of the tumor into the left orbit led to the decision of an external endoscopic approach. We considered that a possible CSF leak at the posterior wall of the right frontal sinus, as well as an important intra-operative bleeding, cannot be managed properly by a trans-nasal approach.
We underwent the surgery using General Anesthesia with OT Intubation. Although the tumor was large (horizontal diameter – 82mm, antero-posterior – 18mm, vertical – 43mm), we decided that the approach should be performed by the midline of the glabella, through a bone window that would allow the access of a telescope with a 4 mm diameter plus 2 other tools (suction tube + endoscopic forceps or a 2mm microdebrider). Skin incision: 20mm, bone fenestration with 13mm horizontal diameter and 10mm vertical diameter.
A hard tumor is shown upon palpation, with a macroscopic aspect of an inverted papilloma, well-vascularized, that occupies both frontal sinuses and dives through the nasofrontal ducts in the anterior ethmoidal cells. The apparent origin of the tumor is located at the junction between the posterior wall of the left frontal sinus and the intersinusal septum, in the upper floor of the sinus cavity.
Although the approach was carried out through a small hole, using the 300, 700 and 900 angled optics and the angled tools (Heuwieser forceps of 700 and 900, angled suction tube and a monopolar malleable suction cautery), we achieved a full-macroscopic abaltion using „piece-meal” method. There is a partial exposure of the dura mater and the left orbital periosteum, but there is no signs of penetration at their level. A Draf II trans-nasal endoscopic approach is performed for the restoration of ventilation in both frontal sinuses. Radiofrequency hemostasis – fulfuration 10W. Efficient hemostasis, does not require nasal package. The integrity of the bone support is restored using a titanium mash fixed with biocompatible screws (fig. 2). Intradermal skinsuture (Vicryl 5.0).
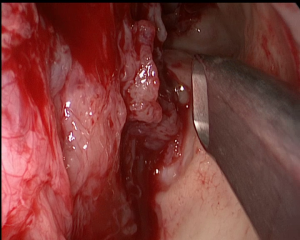

Fig. 2: intraoperatory macroscopic aspect –700optics
Restoration of bone support using Titanium mash
A CT scan using a contrast substance is performed at the end of the surgery (fig. 3). It confirms the complete macroscopic resection of the tumor and a wide ventilation of both frontal sinuses.Although macroscopically the appearance suggests an inverted papilloma, IHC examination of the resected piece describes tissue fragments covered by a respiratory type epithelium, with edema-like stroma with abundant chronic inflammatory infiltrate adding eosinophils and normal-looking glandular structures. IHC reveals the diagnosis of a glandular subtype of sinus inflammatory polyp.
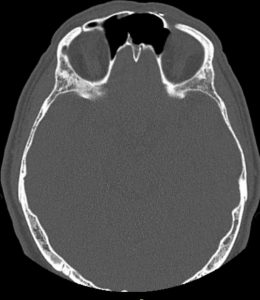
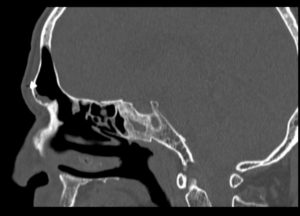
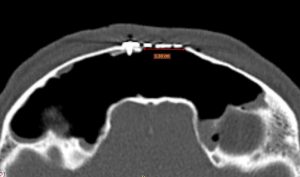
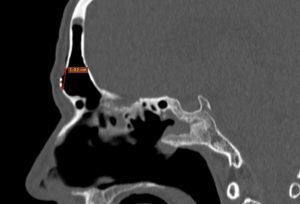
Fig. 3: Up: CT postoperatory aspect axial, sagital.
down:lenghts of bone brace: 13mm/10mm
We have presented this case to point out that there are many situations when the pathology of the frontal sinuses still requires an external approach, even when we consider that the surgical team has a strong experience in trans-nasal endoscopic surgery. The peculiarity of the case was the small bone-window through which the tumor was resected, the advantage we had being given by the usage of optics and angular tools that made the resection complete and safe for the patient.
CSF leaks, the frontal sinus osteomas that exceed the diameter of the nasofrontal duct and large solid tumors, can be safely managed for the patient through a minimally invasive transcranial endoscopic approach that is lesion-centered.
This article does not contain any bibliographical references since it describes a strictly personal experience of the authors.